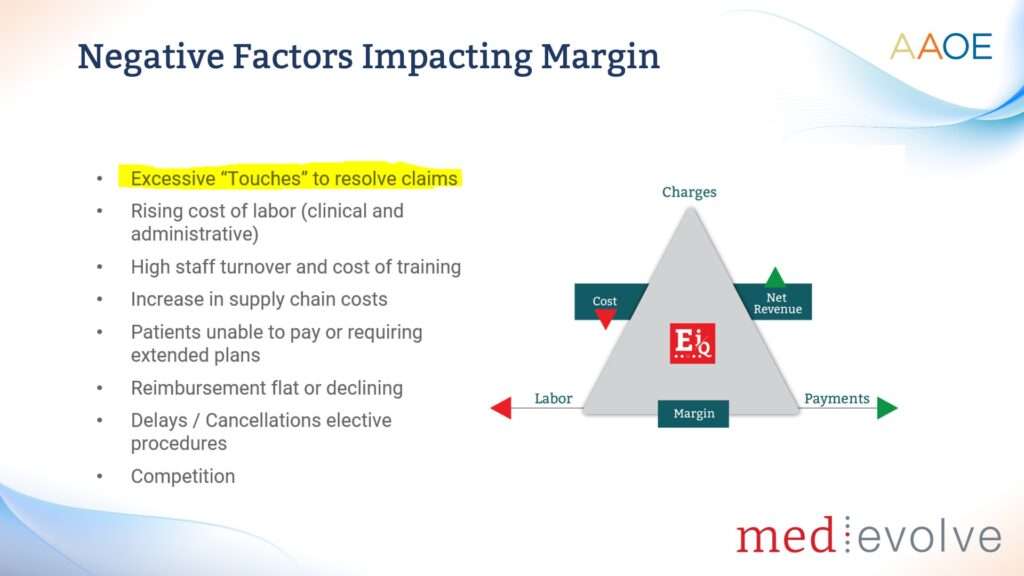
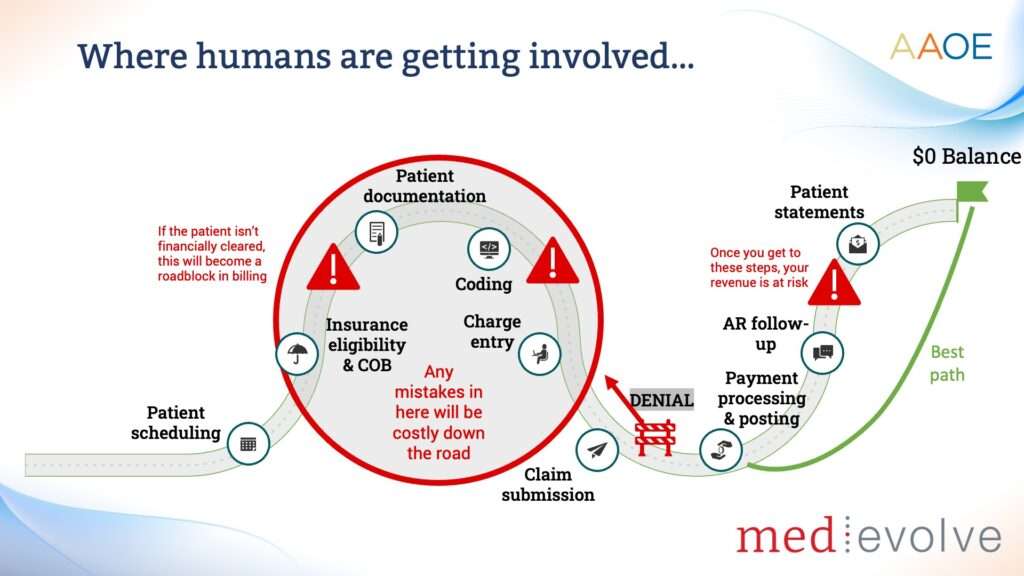
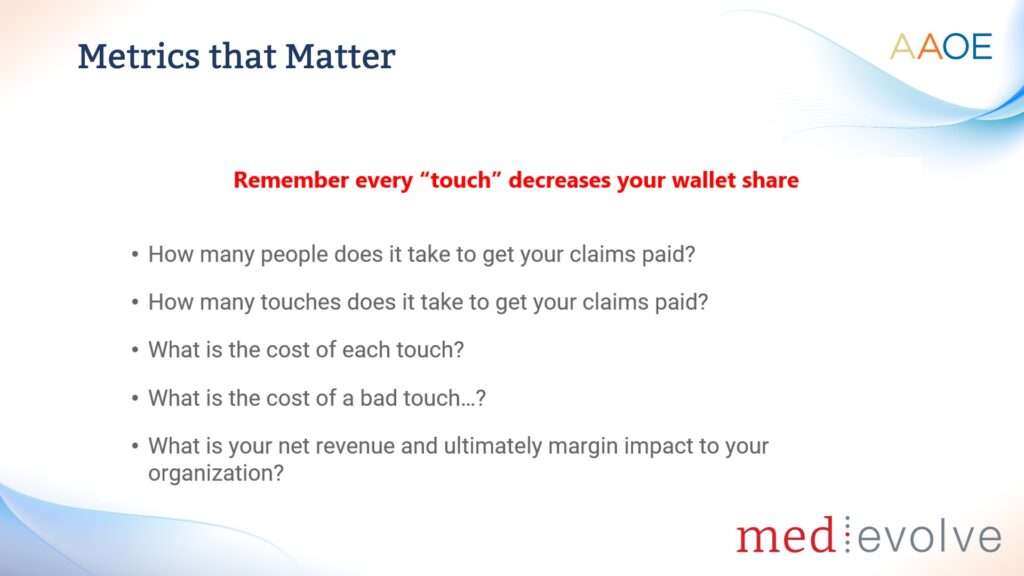
Healthcare Connections Podcast: The Cost of Wasted Touches – Rethinking Revenue Cycle Management in Healthcare
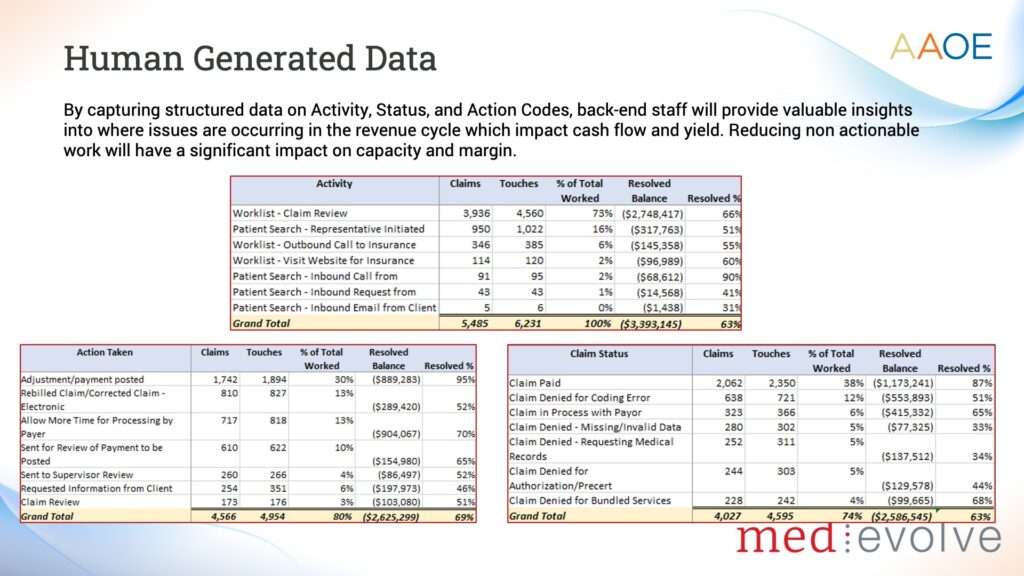
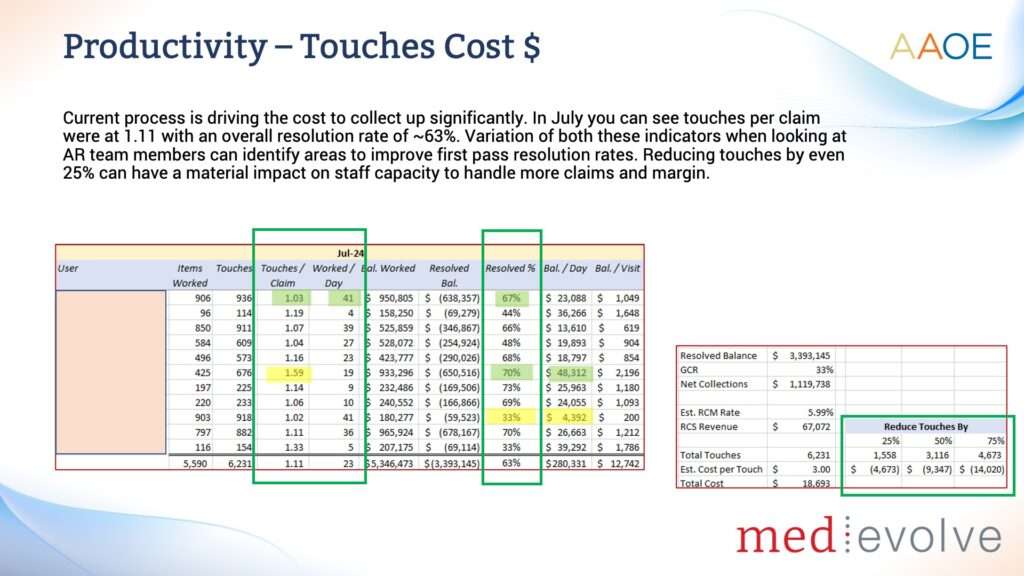
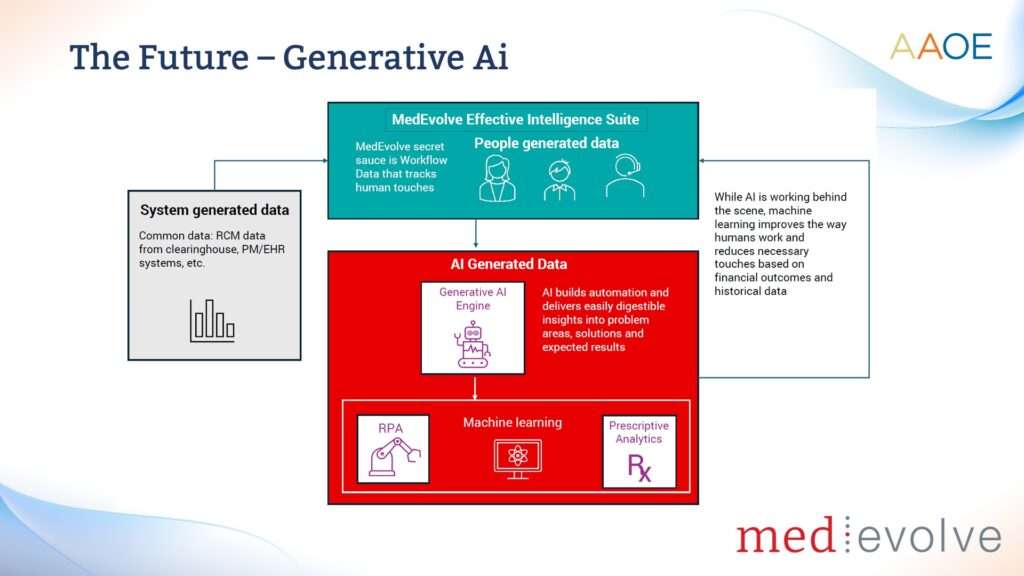
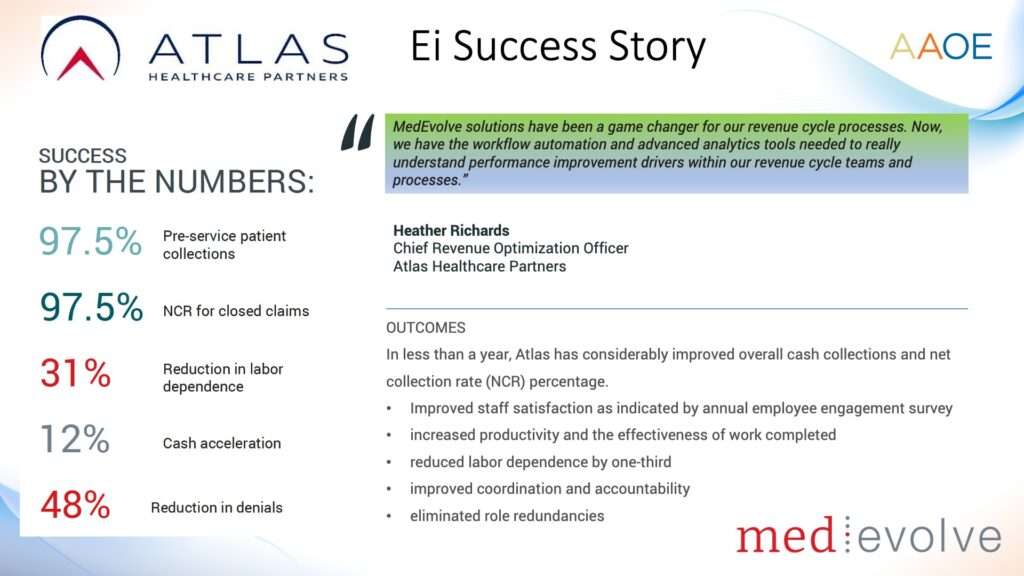
Host Jeremy Winn speaks with Matt Seefeld, CEO of Medevolve, about the challenges and opportunities in healthcare revenue cycle management.