Review and assess your practice’s financial status in 5 min or less and know exact where you are losing money and why. Measure the work effort of every revenue cycle employee, incentivize and retain your top performers, and help employees that need improvement.
You can prevent most common denials, rejections and write-offs during the scheduling and pre-registration process in advance of the appointment. Configure checkpoints and use central task management to quickly clear patients and keep your front office staffing needs at a minimum.
Aligning the power of the MedEvolve Coding solutions with your internal resources personalizes and trains the autonomous coding model, increasing the speed that auto-codes are generated. The portal workflow also drives operational efficiency, resulting in repeatable and scalable performance.
As team members log in to the web-based application and record each “touch” of a claim, outcome, and next task, key data points are recorded like who completed the task and when, outcome, task notes, internal / external messages sent, collection success and other data points that feed into our real-time analytics.
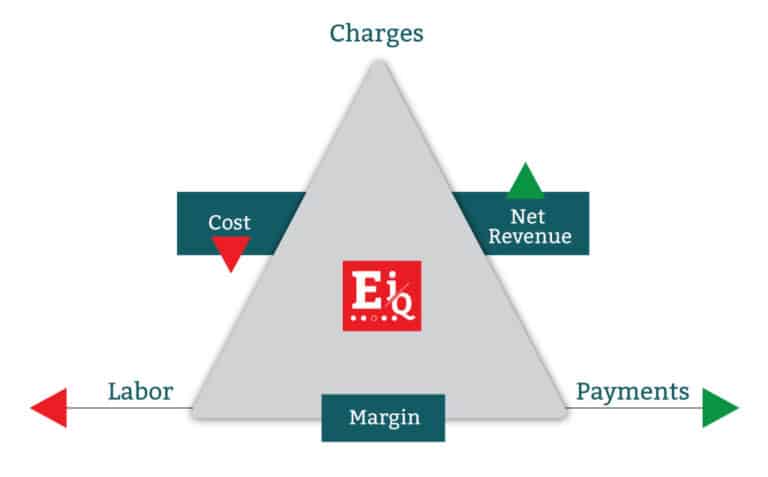
Reduce RCM labor dependency with workflow automation, task management, & real-time analytics to increase margin.
Outsource your medical billing to us with over 20 years of revenue cycle experience incorporating Effective Intelligence in house.
Improve patient collection rates with account resolution services: call center, mobile engagement, payment portal & counseling.
Increase productivity and visibility into front & back office processes while keeping your staff focused.
Monday – Friday
7:00 am – 7:00pm
1115 West 3rd Street
Little Rock, AR 72201
Privacy Policy | 2024 All Rights Reserved