Columbia Orthopedic Group Transitions to a Remote Workforce with RCM Automation & Task Management
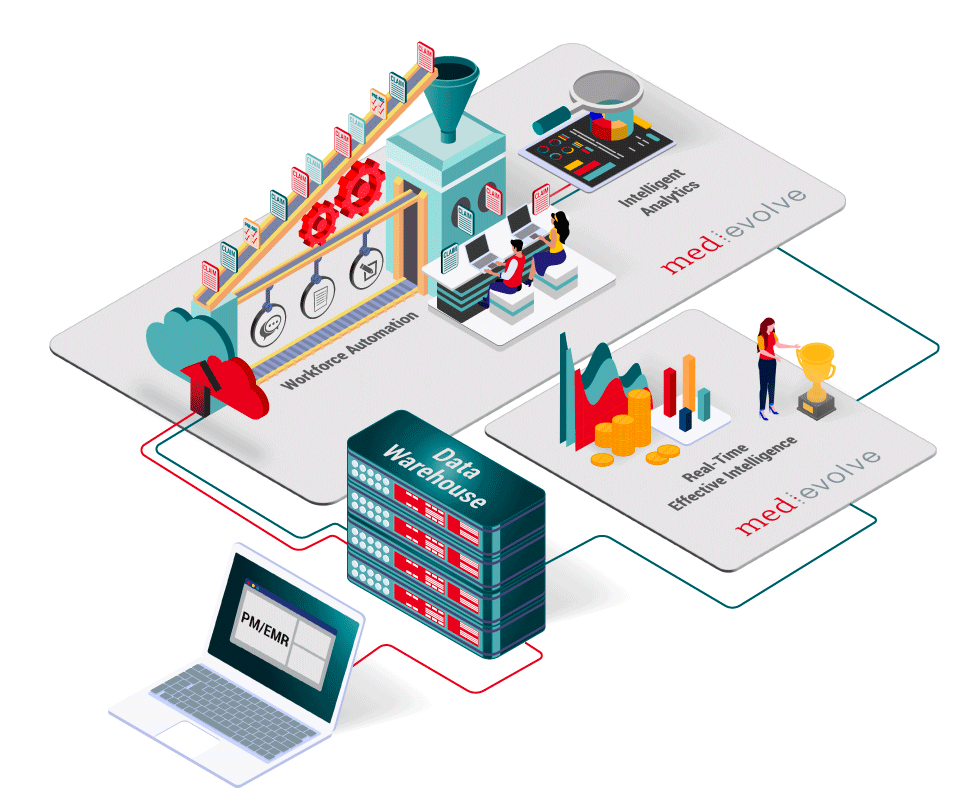
Using Medevolve Effective Intelligence, Columbia Orthopedics was able to measure staff productivity during the pandemic & measure work effort in real time.